
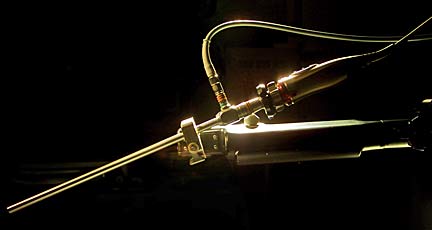
Dr. Randal Aaberg of Kaiser Permanente, above, uses a one-armed robot to perform laparoscopic surgery on prostate cancer patients. Aaberg's image was captured by the camera on the laparoscope and displayed on a monitor, similar to the way he sees where the robot is going during surgery.
New tool in
cancer fight
Laparoscopy joins radiation
and conventional surgery
as prostate treatments
A minimally invasive procedure is available in Hawaii as a new option to treat prostate cancer, the most common cancer in men.
"You can't underestimate the difference for a person," said Dr. Randal Aaberg, urologist at Kaiser Moanalua Medical Center. "If someone leaves the hospital looking like they had a haircut instead of being run over by a truck, it makes a big difference."
Aaberg and Dr. Mark Yamamura have done up to 150 laparoscopic prostate surgeries at Kaiser since February 2003.
Drs. Charles Kim and David Wei teamed up about a year ago to perform the surgery at Kuakini Medical Center, and they've done about 40 procedures.
"It's usually reserved for younger men with localized prostate cancer who we think have a high chance for a cure with surgery," Kim said.
The doctors said anywhere from one in six to one in 10 men will get cancer of the prostate, a walnut-shaped gland near the bladder and rectum and surrounding the urethra.
Men over age 50 should be screened annually for prostate cancer and those considered at risk should begin getting tested at age 40, the doctors advise.
Prostate cancer is being diagnosed earlier because of the prostate-specific antigen test and digital rectal examination. The PSA test has some shortcomings but is considered the best available for prostate screening.
Laparoscopic, or "keyhole," surgery is one of many ways of treating the cancer. It involves making five small incisions in the lower abdomen. Traditional "open" surgery involves a six- to 10-inch incision down the center of the abdomen, although two Hawaii doctors have it down to about three inches.
Patients have less bleeding during laparoscopic surgery, they leave the hospital in one or two days and have less pain, the doctors said.
Urinary incontinence and impotence are two big concerns after traditional surgery. So far, they appear to be the same after laparoscopic surgery, Aaberg said.
But he said, "If you can offer someone less invasive surgery with the same results, it comes out a great victory."
Kim said the surgeons have "a very, very good view of the prostate and surrounding organs with laparoscopy." This enables them to do a better dissection, resulting in "remarkably less" pain for patients and faster recovery, he said.
Aaberg and Yamamura use a one-armed robot that holds the tiny camera. They guide it to put the camera where they want to work.
Aaberg believes better visualization with the camera in removing the prostate will be helpful in sparing nearby nerves involved in sexual function.
He said he suspects, "we will see a benefit with erections ... if we watch long enough and measure our results carefully enough."
Many mainland doctors are using a $1.3 million robot with three arms controlled by the surgeon with joysticks. Aaberg said the three arms are kind of bulky. He prefers the one-armed robot because he likes the "tactile feedback, to be able to feel and know what I'm doing."
Minimally invasive surgery for prostate removal was first done in Texas in the late 1990s, but it was an arduous procedure, patients didn't do well and it was abandoned. Persisting with the technique, French surgeons performed a series of surgeries that did well and they have taught others.
"There's a big revival of interest; everyone's trying to learn how to do laparoscopic prostates," said Dr. Herbert K.W. Chinn, who did the first two at the Queen's Medical Center, one with Charles Kim and the other with a mainland leader in the field. Kim and Aaberg also worked initially with mainland specialists in laparoscopic prostactectomies.

Drs. Charles Kim, left and David Wei, along with registered nurse Carrie Mak perform laparoscopic prostate surgeries at Kuakini Medical Center.
He said he does the procedure in a way that has greatly increased the continence rate. And he and his brother, Dr. Stephen K.B. Chinn of Straub Clinic & Hospital, have pared the incision to a bikini line of little more than three inches, he said.
Dr. Al Mariani, Kaiser Permanente chief of surgery in urology, said laparoscopic surgery is "very difficult and demanding." And there is a lot of controversy as to whether surgery is better than radiation for prostate cancer, he said. "It's not completely resolved because there aren't any good randomized control studies.
"Advocates of surgery, and I think they're right, would say with surgery you have a chance of getting the tumor completely out of the body. With radiation, there seems to be a high probability of radioresistant cancer cells. Whether these will grow and kill the patient during expected lifetime is unclear."
Prostate cancer is slow growing and potentially curable, Mariani said. "Even when it has spread, treatments are effective for long periods of time, months to years even for advanced cancer, not weeks to months."
"The laparoscopic stuff sounds very sexy," said Dr. John Lederer, medical director of the Queen's Medical Center's Nae'a Radiation Oncology Department.
But "there's no evidence it's better treatment than what we've got available. In terms of incontinence and potency, seeds are the best option," he said.
Radioactive seeds are another option for prostate cancer patients. They are implanted into the gland to fight the cancer.
Lederer said he has done about 800 radioactive seed implants for prostate cancer in six years, with a success rate of about 95 percent. And he's had no failures in about 250 low-risk cases, he said.
"Until they can prove to me they can get better than 100 percent in six years, I'm a little bit loathe to believe claims.
"The bottom line is it doesn't matter which treatment you pick; you don't know for five or 10 years if you made the right decision," Lederer added. Patients should choose a treatment they're comfortable with that doctors agree is a reasonable option, he said.

|
Surgery relieves
patient’s fears
A Honolulu man chooses
laparoscopy over radiation
to treat his prostate cancer
Francis Kawakami says he's "a worry bug" so he chose to have his prostate removed by laparoscopic surgery when a biopsy showed it was cancerous.
He said the doctor told him, "which was good news in a way," that prostate cancer grows slowly and he could take radiation treatment if the cancer had not spread.
"After they found it was contained, because of my age, for example, if I didn't do anything, it takes perhaps 10 to 15 years ... to spread out. He said I'd probably die of something else."
But the 69-year-old said, "I worry about every little thing. With radiation, I would be worrying every day that cancer was still in my body. I didn't want to worry about that."
Kawakami, who retired in 1995 after 38 years as a technician for the Hawaii Army National Guard, said his family doctor, Michael Mihara, sent him to urologist Stephan Lee to get a biopsy when he noticed his prostate-specific antigen test had gone up significantly.
One sample in the biopsy was cancerous, and the Pacific Palisades resident was referred to Dr. Charles Kim at Kuakini Medical Center.
He had laparoscopic surgery Aug. 31 and was in the hospital three days. "That technology is fabulous," he said.
"If I took regular surgery, they would have to cut right across and it would take a heck of a lot longer. I didn't want that," he said, recalling surgery on his back in 1970. "It was the old way. They cut you open."
He said he was told the surgery would take about six hours but it took only about 4.5 hours. His doctor told him he "contributed to it because I'm skinny," he said.
"Technology has advanced tremendously," Kawakami said, adding that he is "one of the fortunate ones." He had a slight urine drip for about three months after surgery and then it stopped.
Before the surgery, he said he had experienced what's called "the old man's disease," difficulty urinating. Now, he said, "It is a million times easier."
Kawakami said he isn't able to have an erection "but as you get older, it's not so important. I'd much rather go to Vegas and shoot craps.
"My wife and I love each other in many, many other ways. We just celebrated our 50th anniversary last year. Sex is the least of our concerns now. We do everything else together."
He said his wife, Mildred, always goes to doctor appointments with him so both know what's happening.
"I strongly recommend that anybody going towards their senior years go and have a least a minimum annual checkup, a complete blood test, and see a doctor," Kawakami said.
He said his family doctor practices preventive medicine. "I found out that's so important. He catches things before it really happens."
E-mail to City Desk
[News] [Business] [Features] [Sports] [Editorial] [Do It Electric!]
[Classified Ads] [Search] [Subscribe] [Info] [Letter to Editor]
[Feedback]
