Doctors urge state
to reform insurance
High malpractice costs are
hurting isle treatment, they say
Hawaii doctors are limiting or closing practices, refusing emergency calls or leaving the state because of soaring medical malpractice premiums and costly lawsuits, state lawmakers were told yesterday.
At a House Health Committee meeting yesterday, doctors and other health care officials offered strong support for proposed legislation for medical malpractice reform.
"Laymen believe that the emergency room is always ready and doctors are always on call to help. This is no longer true," testified Dr. Russell Stodd of Kahului, Hawaii Medical Association past president and member of the Hawaii Health Systems Corporation board.
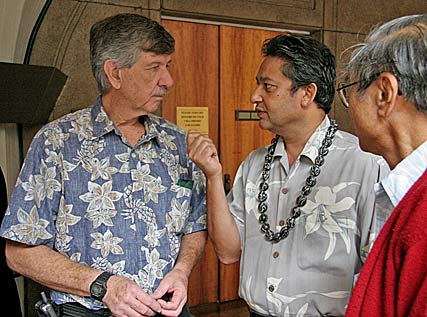
Kauai doctor Gerald McKenna, left, talked yesterday at the state Capitol with Dr. Inam Rahman, president of the Hawaii Medical Association, and Big Island retired surgeon Desmond Wong.
"You really need a big fix," he said, referring to Hawaii's malpractice problems, adding that House Bill 648 is the best of various bills proposed to do it. Among key features:
» A sliding scale would be established for attorneys' fees.
» The amount of the award would be assessed by the percentage of negligence, and joint and several liability would be allowed if a health care provider's negligence was 25 percent or more.
» A three-year statute of limitation would be set to file a medical lawsuit.
He said capping non-economic damages (for pain and suffering) would punish seriously injured people and would not help to increase on-call physicians.
He said he took his 96-year-old mother to the Queen's Medical Center trauma center recently with a broken femur, and she had "terrific" treatment by orthopedic surgeons.
"I think this (bill) would be unnecessary," Toyofuku said.
Health professionals, however, said that public access to health care is threatened.
"It is a crisis," said Dr. Inam Rahman, internal medicine and family practice doctor, who heads the Hawaii Medical Association.
"There will almost be no health care system in two or three years," he said in an interview, referring to escalating medical malpractice costs.
He said the state's only trauma center at Queen's is in trouble because a lot of specialists and primary care physicians have left the state.
"They can't take it anymore," he said.
He said he has a busy practice and is still struggling because of high costs of doing business, fees fixed by insurance coverage and constantly rising malpractice premiums.
His premiums two years ago cost $2,500 a year, he said. Now, he pays that much every three months. When the cost hits $18,000 a year, he will have to close his practice, he said.
"Doctors are really frustrated. It is a nightmare for me," he said.
Rahman said Hawaii has a shortage of neurosurgeons, gastroenterologists, orthopedic surgeons, general surgeons and anesthesiologists. Shortages are most severe on the neighbor islands.
Rahman and Rich Meiers, president and chief executive of the Healthcare Association of Hawaii, said physicians and hospital officials have been meeting to address the issues. They have discussed the seriousness of not having on-call doctors available at the trauma center, Rahman said.
Many doctors are turning down emergency calls in the middle of the night because often they receive no pay, and they have to care for their own patients the next day, Meiers said.
He also noted a lifestyle change that was seen during the nurses strike. Doctors and nurses want to spend more time with their families, he said.
Stan Berry, chief executive of the North Hawaii Community Hospital, said in an interview that there are nights when no neurosurgeon is available at the Queen's trauma center, and it is often difficult to get an orthopedic surgeon when no one is available on the Big Island to take care of a compound fracture.
"We don't know what to do. It takes many phone calls, lots of pleading and cajoling to get things worked out," Berry said.
[News] [Business] [Features] [Sports] [Editorial] [Do It Electric!]
[Classified Ads] [Search] [Subscribe] [Info] [Letter to Editor]
[Feedback]
