

DOCTORS SPECIALIZING in care of older people are in short supply while Hawaii leads the nation in a zooming over-65 population. CRISIS IN ELDERLY CARE
Help Wanted
Geriatrics doctors are in short
supply as Hawaii's leads
the nation in the number
of elderly residentsIsles' population aging faster than rest of U.S
By Helen Altonn
haltonn@starbulletin.comLack of funding to establish geriatric training programs and inadequate reimbursements for doctors caring for older people are among factors causing a shortage of geriatricians, said Dr. Patricia Lanoie Blanchette, University of Hawaii Geriatric Medicine Program director.
A recent $2 million grant from the Donald W. Reynolds Foundation to the John A. Burns Medical School will help with one of those problems.
It will be used to establish a four-year curriculum in geriatrics, to develop residency programs and provide continuing education for practicing physicians.
The John A. Hartford Foundation also awarded the program $450,000 in a three-year renewal grant for the Center of Excellence in Geriatrics. It will be used to ease the shortage of academic geriatricians.
Nora Uyeda also donated part of her mother's estate to the Geriatric Medicine Program in gratitude for care and service given to her mother.A geriatrician is a physician who specializes in caring for older people, teaches and conducts research in aging, just as a pediatrician does for children.
Blanchette said Hawaii has about 25 geriatric specialists statewide. "Unless someone creates a job, there's not likely to be many more.
"You don't see many geriatricians fully trained in very large numbers in fee-for-service medicine because if you're reimbursed per patient, reimbursements are very low."
Because of the huge cost of Medicare and growing numbers of older people, government has reduced reimbursements for service to cut costs, she said.
Geriatricians also do not have a large turnover of patients because it takes a lot longer to see an older person, she said.
Since private practice of geriatric medicine "doesn't sustain itself very well," geriatricians usually are associated with places that pay them salaries, such as hospitals or the Veterans Administration, Blanchette said.
They might not generate a lot of billing income, but they can achieve savings from earlier diagnosis and better management of patients, she said.
It ends up being less expensive if an old person is seen by a geriatrician instead of "a round robin of various specialists who are not well coordinated by each other," she pointed out.
Older people present problems in a different way than a younger person, she said. "You used to hear, 'Oh, they're just normal old people.' You hear it less now than before."
She said geriatric specialists know older people do not tolerate invasive procedures as much as younger people and are able to help them make decisions about limiting them.
"We're comfortable with, not rationing care, but making care appropriately targeted in a very precise way so we don't end up with procedures, given a conscious choice, a person wouldn't want."
Testifying before a U.S. Senate committee in June, Howard Fillit, senior associate of the International Longevity Center-USA, said 2,400 academic geriatricians are needed to prepare physicians for the aging population.
Yet fewer than 600 faculty members nationally now list geriatrics as their medical specialty, he said.
He urged funding to prepare for the retirement of the baby-boom generation, stressing, "One effective, low-cost way to improve the health and quality of life of older Americans is to develop a cadre of academic geriatricians to educate all physicians in geriatrics."
Physicians trained in internal medicine or family practice who take an additional one or two years of training to specialize in geriatrics are called fellows.
Blanchette said the UH medical school has one of the largest geriatrics training programs in the country, with a total of 12 positions for fellows tied with very large schools or centers on the mainland.
The program, based at Kuakini Medical Center, has a three-month wait list for patients. It would be longer, but that is all the program will take, Blanchette said. "I get irate calls from people."
Kuakini for a long time has been committed to caring for older people and was doing it "before others even saw the need," Blanchette said.
Hawaii is aging far more rapidly than the rest of the nation, says the International Longevity Center-USA, a New York-based nonprofit research and education organization. Isles’ population aging
faster than rest of
U.S., study findsBy Helen Altonn
haltonn@starbulletin.comThe center prepared a statistical picture of aging of the United States and Hawaii based on 1990 and 2000 census data.
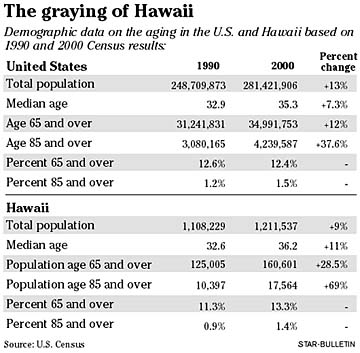
It shows Hawaii had a 69 percent increase in residents over age 85, far exceeding the average increase nationally of 37.6 percent. Hawaii's age 65-and-over population increased 28.5 percent, compared with a 12 percent increase in that population nationally.
The median age in Hawaii in the 2000 census was 36.2 -- ninth highest of all states. It was 32.6 in 1990. Nationally, the median age was 35.3 in the latest census, compared with 32.9 in 1990.
Hawaii's total population in 2000 was 1,211,537, a 9 percent increase in 10 years. The age 65-and-over population numbered 160,601, compared with 125,005 in 1990.
Those 85 and over numbered 17,564 in 2000, leaping from 10,397 in 1990. In 2015 when baby boomers begin to retire, according to the Census Bureau, the population over 65 nationally will jump to 46 million -- 15 percent of the total population, the Longevity Center said.
By 2050 the United States is expected to have more than 80 million people over age 65, about 20 percent of the population.