

Alternative to
hysterectomy gains
popularity here
A less invasive procedure used in
Canada and France lets isle women
avoid major surgeryWhat isle doctors say
By Helen Altonn
Star-BulletinTHE 48-year-old Kailua woman was hemorrhaging so badly last August that she had to be hospitalized.
Cynthia Monsour was suffering from fibroids, benign growths of the uterus that are common in women. They may cause no symptoms, minor symptoms -- or heavy menstrual bleeding, clotting and pelvic pain.
Monsour said her bleeding was so heavy at times that she couldn't leave home.
She refused a transfusion for anemia, fearing she would have a heart attack or stroke because of her low blood count, she said.
She also fought against a hysterectomy to remove her uterus, the most common treatment for uterine fibroids.

Fibroids account for about a third of the more than a half million hysterectomies performed annually in the United States, according to the Society of Cardiovascular & Interventional Radiology."Women are too quick to be under the knife because a doctor recommends a hysterectomy," Monsour said. "The business of the day is, 'Just take this out.' "
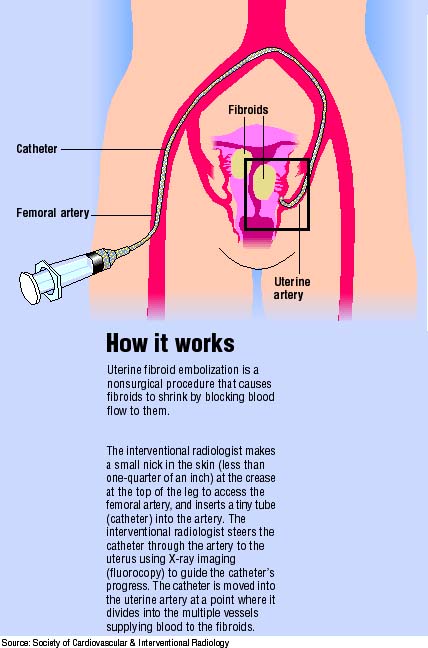
In two years of research on alternatives, she learned about a new procedure in the United States -- uterine fibroid embolization.
It involves blocking arteries that supply blood to the fibroids, which causes them to shrink.
It's a minimally invasive technique done on an outpatient or overnight basis. "You can go back to your normal schedule within weeks," Monsour said. "With a hysterectomy, aside from mental repair, it takes six weeks to repair physically."
She had to fight the Hawaii Medical Service Association for six months to get approval for the procedure, she said.
"They kept insisting I had to have a hysterectomy. I kept asking, 'Who was making these decisions for me?' "
'We don't just castrate, do we?' Cynthia Monsour
PATIENT WHO FOUGHT FOR A
LESS INVASIVE OPTION WHEN INSURERS WOULD
ONLY SUPPORT REMOVING
HER UTERUSShe filed two appeals: "The second time, I asked them to advise me if I needed legal counsel because I was going to continue.
"I was trying to make them understand I was not trying to avoid surgery but to stay whole. They were not going to force me into a radical hysterectomy."
Dr. Susan Chapman, Monsour's obstetrician/gynecologist, said she discussed all the options with Monsour before deciding on embolization.
They didn't think the procedure was being done in Hawaii so they sought approval for Monsour to go to UCLA, where it started in the United States.
Monsour said HMSA approved the procedure in late June and located Dr. Chuong Nguyen, an interventional radiologist, to perform it Aug. 12.
It was the first such case at Castle Medical Center. "I came through it great," Monsour said.
Nguyen said the technique is practiced in France and Canada but it still isn't widespread in the United States. He began doing it last year at McGill University in Montreal.
He said it's usually done on an outpatient basis but that some patients, like Monsour, may require an overnight stay for pain control. Recovery time is usually a few days to a week, he said.
He said the major risk is the possibility of infection of the uterus, which would lead to a hysterectomy.
Because of that, he said he'd be reluctant to perform the procedure on a young woman who hasn't had children.Although women have become pregnant after the procedure, he said the long-term effect on fertility isn't known.
With older women, he said he would "just wait it out" because fibroids tend to shrink with menopause.
Monsour said she had "really intense pain" immediately after the surgery, and "the weekend was a crisis period for infection to the uterus."
But she was "back to myself" by Aug. 16, she said. She has returned to her part-time job at State Farm Insurance in Kailua. She also is a full-time Hawaii Pacific University student in corporate communications.
Chapman said a hysterectomy may be the best decision for some women, but they must be given options.
"If we've gone through all the alternatives and that's best for her, the patient can go into a hysterectomy with a more settled mind," she said.
Some patients who have less invasive procedures also may end up at some time with a hysterectomy, added Chapman, who specializes in minimally invasive surgery. "But at least you'll know you tried some other things."
She said a lesser procedure could be done to control pain and bleeding temporarily for some patients if timing is bad for major surgery.
"Most women in Hawaii work," the physician said. "They have kids and elderly parents to care for. It's not like they can put their feet up for six weeks and recover from major surgery."
Monsour has three children, including two daughters. Her message to them and other women is not to agree automatically with a surgeon recommending a hysterectomy. She urges women to examine the alternatives and insist that their insurance carrier cover the embolization procedure if it is a viable option.
"We don't just castrate, do we?" she said. "The mentality of some doctors is, the easiest thing to do is just get rid of it (the uterus). ... That's really old mentality. We need to get rid of that."
Patients opting for new
By Helen Altonn
method call it fantastic,
isle doctor says
Star-BulletinFIBROID tumors of the uterus can grow to the size of a basketball and make a woman look like she's five months or more pregnant.
But symptoms aren't necessarily related to the size of the fibroids, said Dr. Peter Abcarian, Kaiser Permanente interventional radiologist.
Some relatively small fibroids have more symptoms than massive fibroids have, he said, noting that their location may be a factor.
Symptoms include bleeding and pain and, if the fibroids are bulky, they can cause pelvic discomfort and press on the bladder so the woman has to urinate every 30 to 60 minutes, Abcarian said.
He said uterine fibroids "are extremely common -- 30 to 40 percent of women will have them by age 40."
Abcarian says Kaiser Medical Center was the first hospital in Hawaii to offer uterine fibroid embolization, a nonsurgical procedure that causes fibroids to shrink.
Dr. Scott Goodwin of UCLA reported the first successful cases of fibroid embolization in the United States in mid-1997.
Abcarian said he began embolizing, or blocking, the blood flow to uterine arteries in emergencies in 1997 and began fibroid embolizations in early 1998. He has since had about 20 cases, he said.
When the technique wasn't available at other hospitals, Abcarian said he received calls regularly from women covered by HMSA asking him to do the procedure. "We've done it for one person with HMSA coverage after about six months of hurdles."
Other hospitals have since started offering the technique, performed by interventional radiologists, Abcarian said.
He said he works with two physicians at Tripler Army Medical Hospital, which began offering the procedure after Kaiser.
The Queen's Medical Center began offering it in January. And Castle Medical Center had its first case this month.
"This is a new alternative to hysterectomy," said Queen's interventional radiologist John Chan. "If they have the option, I think a lot of women will opt for this. ... If it fails, you really haven't lost any ground. You have a backup alternative, which is a hysterectomy."
Chan said the embolization procedure is less invasive, has a shorter recovery period, is very effective, "and women still have their uterus."
"On the other hand," he said, "if you still have the organ, you are susceptible later on in life to developing diseases related to the organ, whereas a hysterectomy removes that chance."
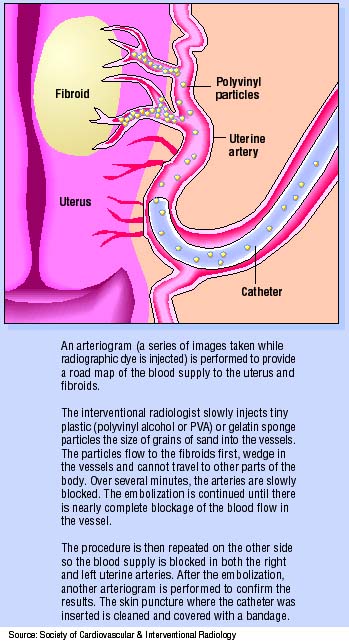
French interventional radiologists developed the procedure in the early 1990s, Abcarian said. They discovered the tumors were shrinking 60 to 80 percent and bleeding symptoms had completely stopped, he said.
"In follow-up studies, the uterus was alive and well."
Chan said the French data is promising. Some women who had the procedure became pregnant and had normal deliveries, he said. "But I think in the U.S. we're slow to adopt things until we get more and more numbers."
Abcarian said he's had "a zero complication rate" from his cases, mostly treated as outpatients. "For most of the women, they say 'fantastic.' "
There still is a concern about longterm effects on fertility, he said, "but the general consensus is it's safe."
Chan said he's had five fibroid embolization cases and he's getting a lot of calls from physicians and patients about the procedure.
"We're screening patients pretty well, working with our gynecologists, to see if they're candidates for this because not all women are," he said. "Currently, we're taking women who do not desire future fertility."
Other options to a hysterectomy, the radiologists said, are drug or hormonal therapies that shrink the fibroids, and a surgical procedure called myomectomy that removes only the fibroids.