

Third appeal
of hospital bill
a charm
Legislation and the Hawaii
Coalition for Health are credited
with helping a Mililani couple
resolve a lengthy medical
insurance disputePatients' rights law might get better
By Helen Altonn
Star-BulletinA Mililani couple's $4,680 hospital bill was paid by their health plan this month after they fought their way through an appeals process that lasted eight months.
Mitch Kaaialii said Queen's Preferred Plan initially denied a claim for hospital costs when his wife, Barbara Ann, became ill while she was pregnant.
The denial was overturned after three appeals.
The Kaaialii case shows how one plan's appeals process works and the possible influence of Hawaii's patients' rights law -- even when its provisions aren't invoked.
The 1998 law provides for an appeal to a three-member panel headed by the insurance commissioner if a patient isn't satisfied after going through a health plan's internal process.
State Insurance Commissioner Wayne Metcalf said, "A number of cases, less than a dozen, have moved from the internal appeals process toward the three-member panel process."So far, however, all have been resolved without having to convene the panel, he said.
He feels "very definitely" that the patients' rights law is contributing to the resolution of medical insurance disputes.
Kaaialii believes the Queen's plan finally paid the hospital bill for his wife July 13 because the next step would have been to go to the insurance commissioner.
But Dr. George Bussey, medical director for the Queen's Medical Center's health plans, said the case was resolved through normal internal appeals procedures.
He said the volume of appeals is low because few things are denied.
And when a decision is overturned, he said it's usually because of additional information, which happened in the Kaaialii case.
Home treatment
Bussey said the hospital bill was denied at the outset based on medical records indicating that home treatment had been used successfully."The issue raised from the plan's side was that she had had successful treatment before on an outpatient basis and there had not been a return to that (before hospitalization) to see if that would help," Bussey said.
Kaaialii said his wife became very dehydrated and suffered severe vomiting in the early stages of pregnancy with their first child, a daughter born May 19.
He said her doctor told them that intravenous fluid treatment at home would help cut health costs. "So we gave it a try to try to save money for the plan."
Pharmacare, which provides home and nutrition services, sent someone to their home to drop off supplies and later sent a nurse to attach the IV and give them general instructions, Kaaialii said.
Home alone
During the day when he was at work, his wife was home alone with no one to monitor her, he said."She had to walk around the house with an IV pole. It just wasn't working. There was always pain at her side. They had to put needles in at different places."
The only times a nurse returned was when his wife called because the IV was hurting or something else was wrong, he said.
Then, he said, it would take at least a couple of hours before a nurse arrived, and his wife would have to remove the IV herself.
Kaaialii said his wife fell several times because she was dizzy and he "had to run home many times" from his job at a finance company in Waipahu.

'She had to walk around
the house with an IV pole. It just
wasn't working. There was always
pain at her side. They had to put
needles in at different places.'MITCH KAAIALII
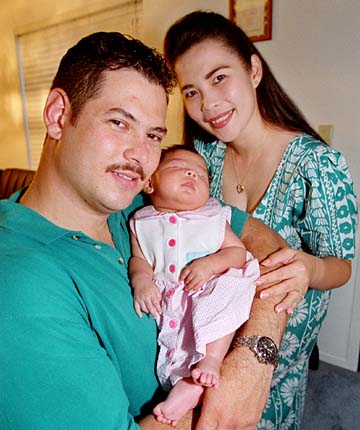
MILILANI RESIDENT, ABOVE, WHO
FINALLY TOOK HIS WIFE, BARBARA ANN, RIGHT, TO
THE HOSPITAL FOR EXTENDED CARE FOR PAIN SHE
WAS EXPERIENCING BEFORE THE BIRTH OF
THEIR DAUGHTER, LAUREN.They started the home treatment the first week of November, but by Nov. 9 they couldn't do it any more, he said. "It was too painful." He took her to the emergency room that night, he said. "I almost had to carry her into Queen's Hospital."
Meanwhile, Pharmacare had listed the home treatment as successful on Barbara Ann's medical record.
Kaaialii said his wife was fine after five days in the hospital but their insurer wouldn't pay the bill, saying hospitalization wasn't necessary, based on Pharmacare's information.
Byron Yoshino, Pharmacare president and chief executive officer, said he had no comment on the case.
Kaaialii said he and his wife's doctor, Elenita Alvarez, wrote several letters to the health plan appealing denial of the hospital payment.
"She was trying to help because it was justified," Kaaialii said. "If it wasn't necessary, I would have paid for it. But that wasn't the case at all. We ended up fighting the thing."
Third opinion
Kaaialii said he was planning to go to the insurance commissioner after two appeals failed. Then Alvarez told him about the Hawaii Coalition for Health.Dr. Arleen Jouxson-Meyers, coalition president, reviewed the case and said "it was just outrageous," Kaaialii said. "We talked to many other doctors, too, and they said there should be no question."
Meyers said the insurance commissioner was willing to take the appeal "but I thought I'd be a good neighbor before I filed it." She said she called the health plan and asked if it wanted to review her analysis and reconsider the denial.
Bussey said a local primary care physician first reviewed the case. The second time it was sent to a group approved for independent outside reviews, and a mainland obstetrician/gynecologist reviewed it. Both upheld the plan's decision.
He said the Kaaialiis, feeling they had exhausted internal reviews, then wanted Meyers to help them file an appeal with the insurance commissioner.
"They were unaware they had a third level of appeal," Bussey said. "Once we got them to understand they had a third level of appeal, the treating physician and family opted to take advantage of that."
A local obstetrician/gynecologist reviewed the records and reversed the earlier decisions. But his action wasn't based on the records as much as on what Kaaialii said about his wife's condition, Bussey said.
"He (the doctor) said if you look at the medical record, it (treatment) might have been something done on an outpatient basis. If you listen to the husband about how his wife was doing, it would be equally reasonable to admit her to the hospital."
Kaaialii feels the coalition facilitated the reversal.
When Meyers got involved, he said, "It happened real fast."
But Bussey said, "We didn't do anything unique in this case, except when Dr. Meyers started talking about the insurance commissioner, we said, 'Excuse us, you have one more step to go.' "
Bussey said the Queen's health plans supported passage of the patients' rights bill because "it puts into law what we do already for the most part."
State’s patients’ rights
By Helen Altonn
law might get better
Star-BulletinA task force appointed by the insurance commissioner is looking at ways to improve a law that already puts Hawaii ahead of most states, health officials say. It's a patients' rights law drafted by Hawaii health-care representatives and passed by the Legislature last year.
"It reflects community consensus. It wasn't as politicized, at least the discussion wasn't, as it appears to be in Washington," said Clifford Cisco, Hawaii Medical Service Association senior vice president.
"It is just another example of Hawaii leading the way," he said.
Health officials here are comparing Hawaii's law to patients' rights legislation in Congress and waiting to see what happens, Cisco said.
As a consumer group, the Hawaii Coalition for Health prefers the Democratic version, which is similar to Hawaii's law, said Dr. Arleen-Jouxson Meyers, president.
The Democratic bill provides for an independent review process for appeals, while the GOP bill calls for a review panel appointed by the health plan.
Under Hawaii's law, a patient who isn't satisfied with the results of a health plan's appeals process can go to the insurance commissioner. A panel headed by the commissioner, with representatives from a health-care plan and the medical speciality involved, will hear such cases.
Insurance Commissioner Wayne Metcalf also has asked the Patient Rights and Responsibilities Task Force to work on standards for the internal appeals process in Hawaii's health plans.
Many had no appeals procedures until a few years ago when Medicare imposed rules requiring them, Meyers said. But there are no guidelines, and the process varies from plan to plan, she said.
"The process can be so cumbersome that it exhausts both the physician and patient (and) they just throw in the towel," she added.
The plans are required by federal law to have at least two tiers of review, and some go further.
The Queen's Medical Center's plans, for example, have three levels of appeal.
The Hawaii Medical Service Association, the state's largest health-care insurer, has two levels of appeal. And if they don't settle the case, it can go to arbitration, Cisco said.
Health plan credentialing organizations also have strict guidelines about appeals processes and are expected to be here next month to meet with the task force, Meyers said.
Metcalf said the Legislature also took an important step in Hawaii's patients' rights bill in bringing health insurance plans under the insurance code with respect to unfair business practices.
The plans, or mutual benefit societies, formerly were covered by only one paragraph in the law, he said. "They were not subject to much of any regulation at the state level."
The Hawaii Coalition for Health would like to see patients able to sue health plans for negligent decisions. House Democrats had that provision in their bill, but it was killed in the Senate.
Under the federal Employment Retirement Income Security Act of 1974, patients covered by an employer-purchased health plan can't sue the plan for malpractice.
"As long as we don't have a federal law, like the Democratic bill, that permits patients to sue a health plan, they still won't be able to hold the health insurer accountable for negligent decision-making," Meyers said.
In a case about a year ago, the 9th Circuit Court of Appeals said just because an employer buys health insurance for employees, it doesn't mean it falls under the Employment Retirement Income Security Act, she said.
"So if somebody tried to sue a health plan in Hawaii, it may not be thrown out of court. No one has tried to do that.
"It's much more beneficial to the entire community if one can resolve disputes through an appeals procedure and not have to sue," Meyers said. "But a patient needs the option to sue, to hold plans more accountable."